Office Hours
| Monday | 9am | 6pm |
| Tuesday | 1pm | 6pm |
| Wednesday | 9am | 6pm |
| Thursday | 9am | 6pm |
| Friday | Closed | |
| Office closed daily for lunch from 12:45pm - 2pm | ||
A migraine usually is a throbbing headache that occurs on one or both sides of the head. The headache typically is accompanied by nausea, vomiting or loss of appetite. Interestingly enough, there are at least 100 types of headaches defined by the International Headache Society, so not every severe headache is a migraine! Migraines can be triggered by certain activities, foods, smells or emotions. Some people are more likely to experience migraines when they are under stress, while others develop migraines when stress is relieved (for example, the day after exams or an important meeting). Conservative management may be effective for controlling symptoms of migraines and reducing their frequency.
A study was performed at the Chiropractic Research Center of Macquarie University that proved that spinal manipulation does in fact help migraines. One hundred seventy-seven volunteers who had migraines for more than 18 years on average were used for the study. The volunteers who received spinal manipulation showed a statistically significant improvement in migraine frequency, duration and disability. Those who received manipulation were also able to considerably reduce the amount of medication they were taking, some eliminating the use of medication altogether.
Temporal Mandibular Joint (TMJ) is the joint between the jaw or mandible and the skull. It is used every time we chew, talk, or even swallow. Its anatomy, as well as its movement, is very complex. There are significant functional relationships between the TMJ and cranio-cervical (head and neck) neuromuscular systems and these can often become dysfunctional (TMD). This dysfunction can cause pain in the jaw or face, popping or clicking during chewing, limitation of jaw movement or headaches. The muscles involved in TMD are frequently an untreated factor in patients with headaches that may have failed other forms of treatment.
The doctors at Charleston Chiropractic Company are highly trained in the evaluation and treatment of this orofacial condition. Our conservative approach to temporomandibular dysfunction consists of a detailed examination of the TMJ and its function, as well as the function of the cervical spine (neck). Treatment focuses on releasing the tension with the proper soft tissue treatments, in some cases mobilizing the jaw or manipulating the neck. Patients are engaged in an active care model that works on how to retrain proper jaw motion with rehabilitation exercises. The goal of this treatment is to restore proper function of the joint and stabilize its motion.
Cervicogenic headaches occur when joints and/or muscles are dysfunctional in the neck. This can cause pain in the head from a variety of sources: Compression of nerves that innervate the head, Referred pain into the head from the neck from tight muscles, Referred pain into the head from joints in the neck that are not moving properly. Upon physical examination, it can be easily determined if this is the cause of your head pain. Once diagnosed, comprehensive treatment to eliminate the cause of the pain can yield highly successful outcomes.
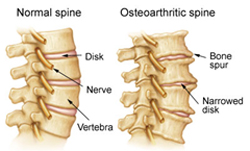
Arthritis has been used to describe chronic irritation, inflammation and degeneration of a joint. However, arthritis is broken up into two groups: inflammatory and degenerative. Inflammatory arthritis produces excessive swelling of the joint and can lead to pain and erosive changes in the joint if left unchecked.
Degenerative arthritis, as the name implies, is a wearing down of the cartilage used to protect the joint. While this does not produce any significant swelling, pain will occur through the friction that occurs when the cartilage has worn away and liberation to the joint is lost.
The degenerative changes will cause stiffness in the joint, which is worsened with waking up in the morning due to lack of movement to the area overnight.
The goal of treating degenerative arthritis is therefore to increase flexibility, joint mobility, and improve surrounding musculature function to the area without further irritation. The goal of treating inflammatory arthritis is, first and foremost, to temporarily reduce inflammation to the area, followed by a plan for helping to prevent the inflammation from re-occurring. As arthritis patients will have pain in the surrounding tissue, a therapeutic plan should be addressed to lend relief and support of the affected area. Conservative treatment can have profound effects on decreasing symptoms and improving function.
Arm pain from a cervical herniated disc is one of the more common cervical spine conditions treated by spine specialists. It usually develops in the 30 to 50-year-old age group.
Although a herniated disk may originate from some sort of trauma or injury to the cervical spine, the symptoms commonly start spontaneously. The arm pain from a cervical herniated disc results because the herniated disc material pinches or presses on a cervical nerve, causing pain to radiate along the nerve pathway down the arm. Along with the pain, numbness and tingling can be present down the arm and into the fingertips. Muscle weakness may also be present.
The two most common levels in the cervical spine to herniate are the C5 – C6 level (cervical 5 and cervical 6) and the C6 – C7 level. The next most common is the C4 – C5 level, and rarely the C7 – T1 level may herniate. The nerve that is affected by the disc herniation is the one exiting the spine at that level, so at the C5 – C6 level, it is the C6 nerve root that is affected.
Symptoms: A cervical herniated disc will typically cause pain patterns and neurological deficits as follows:
It is important to note that the above list comprises typical pain patterns, but they are not absolute. Some people are simply wired up differently than others, and therefore their symptoms are different.
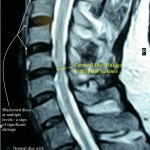
Since there is not a lot of disc material between the vertebral bodies in the cervical spine, the discs are usually not very large. However, the space available for the nerves is also not that great, which means that even a small disc herniation may impinge on the nerve and cause significant pain.
The pain is usually most severe as the nerve first becomes pinched. The majority of the time, the pain from a cervical herniated disc can be controlled with conservative (non-surgical) treatments alone, which is enough to resolve the condition.
Once the pain does start to improve, it is unlikely to return, although it may take longer for the weakness and numbness/tingling to improve. If the pain gets better, it is acceptable to continue with conservative treatment, as there really is no literature that supports the theory that surgery helps the nerve root heal quicker.
All treatments for a cervical herniated disc are essentially designed to help resolve the pain and neurologic symptoms, and improve function.
Mechanical neck and back pain implies the source of pain is in the spine and/or its supporting structure. This occurs when one of the joints in the spine loses its normal joint play (resiliency and shock absorption). It is detected through motion palpation, a procedure in which the doctor gently moves the joint in different directions and assesses its joint play. When a joint develops dysfunction, its normal range of movement may be affected and it can become painful. In addition, joint dysfunction can lead to a muscle imbalance and muscle pain and a vicious cycle:

Any joint of the spine, from the neck all the way down to the sacroiliac joints, can cause mechanical pain. Joints are designed to move and when they do not, pain and degeneration occurs. Conservative treatment is designed for maximizing motion, improving flexibility and finally maximizing muscular coordination, endurance and strength.
Mechanical neck pain can not only create local neck symptoms but also symptoms into the shoulders and upper extremities, as well as headaches. Most people with mechanical back pain experience pain primarily in the lower back. The pain may radiate (spread) to the buttocks, thighs, or knees. Many people may also experience spasms with mechanical back pain. Conservative management and changes in physical activity behavior will typically resolve this condition and can prevent future episodes.
Chiropractors are specialists in treating non-surgical spine injuries and commonly treat whiplash injuries from car accidents. The job of the chiropractor in helping his or her patients overcome the pain and disability associated with whiplash is to:
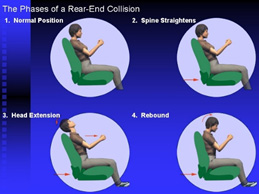
The process of rehabilitation requires a concerted effort between the chiropractor, the patient and any other professional assisting in the case. The likelihood of success is enhanced by a continued focus on restoring normal function. Ninety-three percent of whiplash patients improve with chiropractic care.
The "whiplash"" syndrome is a collection of symptoms produced as a result of soft-tissue injury of the cervical spine. The accumulated literature suggests that 43 percent of patients will suffer long-term symptoms following whiplash injury. If patients are still symptomatic after three months then there is almost a 90 percent chance that they will remain so. No conventional treatment has proven to be effective in these established chronic cases.
A frozen shoulder is a shoulder joint with significant loss of its range of motion in all directions. Long-term immobility of the shoulder joint can put people at risk to develop a frozen shoulder. Frozen shoulder is the result of inflammation, scarring, thickening, and shrinkage of the capsule that surrounds the normal shoulder joint.

There are four muscles that comprise the rotator cuff: Supraspinatus, Infraspinatus, Teres Minor and Subscapularis. A rotator cuff tear is when one of those muscles or the tendon from the muscle is either partially or completely torn. The supraspinatus is the most commonly torn muscle due to its compromised position under the acromonion, or point of the shoulder. While some tears require surgical intervention, the presence of a tear on an MRI or MR Arthrogram does not necessarily mean that surgery is needed, especially in someone over 50 years of age. Some of the most prominent orthopaedic surgeons in the country agree that the symptoms are key in determining the need for surgery. We are able to do a full, comprehensive examination of the shoulder complex to determine the appropriate course of treatment for you. If it is determined by your health care team that surgery is not indicated, then the treatment normally involves functional rehabilitation using Funhab(TM) principles. Kinesio® Taping Method and Graston Technqiue® can also be very effective at treating this condition.
The rotator cuff is a set of four muscles (Supraspinatus, Infraspinatus, Subscapularis, and Teres Minor) that lie over the humeral head in the shoulder that help provide shoulder stability. These muscles can become inflamed and produce shoulder pain. The pain tends to be:
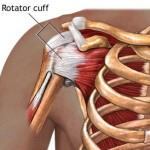
If the pain is severe, it can be difficult to distinguish between rotator cuff tendinitis and a cervical radiculopathy. Tendinitis may be associated with a rotator cuff tear, which can be diagnosed with an MRI scan. Treatment includes conservative treatment to decrease pain and inflammation, improve muscular coordination, identify and correct underlying causes and finally to strengthen the rotator cuff.
If a tear is present, surgery may be necessary to repair the torn muscle/tendon. In many cases, there may be bursa involvement (subacromial bursa), which can cause bursitis. There also may be underlying issues in the cervical and thoracic spine (neck and upper back), which need to be identified and corrected.
A shoulder separation is an injury to the acromioclavicular joint on the top of the shoulder. A shoulder separation occurs where the clavicle and the scapula come together. The two most common descriptions of a shoulder separation are either a direct blow to the shoulder (often seen in football, rugby, or hockey), or a fall on to an outstretched hand (commonly seen after falling off a bicycle or horse).
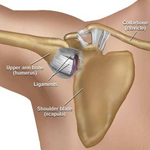
Shoulder dislocations are when the “ball” of the “ball and socket joint” gets forcefully moved out of the “socket” normally through trauma (in sports, a fall, a car accident, etc.). can occur in any direction (front, back, or down), but the most common is the anterior (front) dislocation. A shoulder dislocation can be a very serious injury, especially if it is not able to relocate itself on its own (called spontaneous relocation). In those cases, the patient should go to the nearest emergency room to have the shoulder joint put "back into place."
In other cases, the shoulder muscles need to be specifically strengthened so that they can help to prevent another dislocation. This is best accomplished using Kinesio® Taping Method and Funhab (TM) which strengthen the muscles that are weak and loosen the ones that are too tight. It is also vital that the shoulder blade muscles, called the scapular stabilizers are in the proper balance in order to help position the shoulder in a way that minimizes the risk for injury.
The labrum is a cartilage cuff in the shoulder joint. Depending on where the tear occurs, the pain will present differently. Most commonly, symptoms include an aching in the shoulder joint, clicking or catching of the shoulder with movement, and pain with specific activities. Labral tears are commonly seen in patients who have dislocated their shoulder as well as baseball, volleyball, and tennis players (due to overhead activity). Occasionally, surgery is required to repair the tears, however, ice, stretching, and strengthening exercises can be effective in resolving the problem.
TOS occurs when the nerves and vascular structures from the neck get compressed as they run through the shoulder into the upper extremity. Tests upon physical exam can usually identify the location of the compression. Many times, there may also be compression in the spine or further down the shoulder, elbow, arm or hand. Symptoms may include numbness, t ingling, weakness, pain or blanching of any of the fingers. Conservative management can be very effective in treating TOS without drugs or surgery.
Elbow Epicondylitis/Epicondylosis describes acute and chronic inflammation of the muscles of the forearm that attach at the elbow that become inflamed. The inflammation occurs both at the periosteum (connective tissue covering of the bone) as well as the muscles and tendons that insert on the bone. Many times, the biomechanical problem is in the shoulder and/or wrist. Conservative management in most cases will decrease the pain, improve function and prevent reoccurrences.
TOS occurs when the nerves and vascular structures from the neck get compressed as they run through the shoulder into the upper extremity. Tests upon physical exam can usually identify the location of the compression. Many times, there may also be compression in the spine or further down the shoulder, elbow, arm or hand. Symptoms may include numbness, tingling, weakness, pain or blanching of any of the fingers. Conservative management can be very effective in treating TOS without drugs or surgery.
The carpal tunnel is formed the wrist bones on the bottom and the transverse carpal ligament over the top. The median nerve runs through the tunnel along with the flexor
tendons to the wrist. Pressure within the tunnel can compromise the nerve and lead to carpal tunnel syndrome. The hallmark of carpal tunnel syndrome is numbness in the
thumb, index and middle finger. Additional symptoms can include:
The condition is more common in pregnant women, middle age women, and people with jobs that include daily repetitive hand motions. The condition is diagnosed by a physical exam, as well as a nerve conduction study, an electrical study that measures the length of time that it takes for a signal to cross the carpal tunnel. A delay is indicative of carpal tunnel syndrome. Initial treatment usually consists of conservative physical therapy, contrast baths, nerve-tendon gliding exercises and addressing other potential causes of nerve entrapment (cervical spine, thoracic outlet, pronator teres muscle of the forearm). It’s also important to recognize that these symptoms can also be caused or contributed from problems in the cervical spine, shoulder or elbow and all those regions must be evaluated in order to treat properly.
If the symptoms persist, cortisone injections can be tried. If conservative measures fail, or there is evidence of nerve damage (such as weak thumb muscles or profound numbness), then the carpal tunnel can be released by surgically incising the ligament to give the nerve more room or also done endoscopically.
TOS occurs when the nerves and vascular structures from the neck get compressed as they run through the shoulder into the upper extremity. Tests upon physical exam can usually identify the location of the compression. Many times, there may also be compression in the spine or further down the shoulder, elbow, arm or hand. Symptoms may include numbness, tingling, weakness, pain or blanching of any of the fingers. Conservative management can be very effective in treating TOS without drugs or surgery.
Trigger finger, also known as stenosing tenosynovitis is a condition in which one of your fingers or your thumb catches in a bent position. Your finger or thumb may straighten with a snap – like a trigger being pulled and released. If trigger finger is severe, your finger may become locked in a bent position. Often painful, trigger finger is caused by a narrowing of the sheath that surrounds the tendon in the affected finger. People whose work or hobbies require repetitive gripping actions are more susceptible. Trigger finger is also more common in women than in men, and in anyone with diabetes. Treatment of trigger finger varies depending on the severity. Many patients will respond to conservative treatment including functional rehabilitation and Graston Technique® among others.
Mechanical neck and back pain implies the source of pain is in the spine and/or its supporting structure. This occurs when one of the joints in the spine loses its normal joint play (resiliency and shock absorption). It is detected through motion palpation, a procedure in which the doctor gently moves the joint in different directions and assesses its joint play. When a joint develops dysfunction, its normal range of movement may be affected and it can become painful. In addition, joint dysfunction can lead to a muscle imbalance and muscle pain and a vicious cycle.
The loss of joint play can cause abnormal signals to the nervous system (there are an abundance of nerve receptors in the joint).
The muscles related to that joint can subsequently become tense or, conversely, underactive. The resulting muscle imbalance can place increased stress on the joint, aggravating the joint dysfunction that already exists. Any joint of the spine, from the neck all the way down to the sacroiliac joints, can cause mechanical pain. Joints are designed to move and when they do not, pain and degeneration occurs. Conservative treatment is designed for maximizing motion, improving flexibility and finally maximizing muscular coordination, endurance and strength. Mechanical neck pain can not only create local neck symptoms but also symptoms into the shoulders and upper extremities, as well as headaches. Most people with mechanical back pain experience pain primarily in the lower back. The pain may radiate (spread) to the buttocks, thighs, or knees. Many people may also experience spasms with mechanical back pain. Conservative management and changes in physical activity behavior will typically resolve this condition and can prevent future episodes.
This condition develops over time during periods of bone growth (such as puberty). It occurs when the front of the spine doesn’t grow as fast as the back of the spine and causes healthy, rectangular-shaped vertebrae to become triangular-shaped and wedged together. This causes the thoracic spine to curve more than normal. Patients become stooped forward with a bent-over posture. The ends of your ribs, although not attached to the spine, rest in indentations in the thoracic vertebrae that help support the ribs. Symptoms may include: Pain in the upper back, numbness, pain or tingling from the upper back and around the chest, leg weakness and chest pain.
Compression fractures are caused by trauma to the spine, such as a car accident or fall. Mild to severe pain may be felt in the back, abdominals, arms, and/or legs and worsens with movement. Limitations of movement, swelling, numbness, and tingling may be also present. While severe fractures require surgery, often a combination of rest and conservative treatment is effective in resolving the symptoms and restoring function.
Arthritis has been used to describe chronic irritation, inflammation and degeneration of a joint. However, arthritis is broken up into two groups: inflammatory and degenerative. Inflammatory arthritis produces excessive swelling of the joint and can lead to pain and erosive changes in the joint if left unchecked.
Degenerative arthritis, as the name implies, is a wearing down of the cartilage used to protect the joint. While this does not produce any significant swelling, pain will occur through the friction that occurs when the cartilage has worn away and liberation to the joint is lost. The degenerative changes will cause stiffness the joint, which is worsened with waking up in the morning due to lack of movement to the area overnight.
The goal of treating degenerative arthritis is therefore to increase flexibility, joint mobility, and improve surrounding musculature function to the area without further irritation. The goal of treating inflammatory arthritis is, first and foremost, to temporarily reduce inflammation to the area, followed by a plan for helping to prevent the inflammation from re-occurring. As arthritis patients will have pain in the surrounding tissue, a therapeutic plan should be addressed to lend relief and support of the affected area. Conservative treatment can have profound effects on decreasing symptoms and improving function.
Multiple studies have shown that as many as 50-82% of pregnant women experience low back pain during pregnancy.
Cause
When working properly, the pelvis works like the keystone of a roman arch to distribute weight (this is why arches are so strong). As pregnancy moves along, the rapidly growing baby causes the center of gravity to move dramatically forward. This change in center of gravity puts stress on joins in the lower back and buttocks called the sacroiliac joints. Further, the body starts to produce Relaxin (a hormone that loosens the body to allow for childbirth to happen). The combination of increased stress (pressure) and a hormone causing them to loosen is often what causes the pain. This also causes the piriformis muscle to be overworked and thus painful. Also, many patients decide to lay and sleep on their left side because the Internet (or mom or a friend) tells them they will be more comfortable. Irritation to the piriformis muscle can also cause referred pain into the leg.
Risks?
There are no studies in the scientific literature that show evidence of injury to pregnant patients rom manipulation or other chiropractic and physical therapy treatments (even though as many as 75% of Chiropractors report having treated pregnant patients. Adverse events from manipulation in the non-pregnant patients are also extremely rare.
How we treat these conditions
As with everything, we do a full, functional examination. We then tailor a program specific to each patient’s needs. Often, the pregnant patients require manipulation of the spine (as the pregnancy moves along, this becomes less of a need) with the goal of restoring normal motion to the joints so they stop hurting. Doing a manipulation also helps to decrease pain, relax spastic muscles and help to stop join and disc degeneration and breakdown.
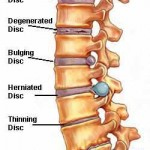
Usually caused by pressure on the sciatic nerve from a herniated disc (also referred to as a bulging disc, ruptured disc). THe problem is often diagnosed as a "radiculopathy," meaning that a disc has protruded from its normal position in the vertebral column and is putting pressure on the nerve (commonly referred to as a pinched nerve). For most people, the pain from sciatica can be severe and debilitating. For others, the pain might be infrequent and irritating, but has the potential to get worse. Usually, sciatica only affects one leg, and the pain radiates through the buttock and/or leg.
One or more of the following sensations may occur:
Any condition that causes irritation or impingement on the sciatic nerve can cause the pain associated with sciatica. The most common cause is herniated disc in the lower back. Other common causes include a narrowing of the spinal canal (where the spinal cord runs), degenerative disc disease or arthritis. Nerve pain is caused by a combination of pressure and inflammation on the nerve root, and treatment is centered on relieving both of these conditions. Conservative treatment is designed to decrease pain and inflammation, improve flexibility of the muscles and mobility of the joints, and to improve muscular function and spinal stability.
Trochanteric bursitis occurs when the fluid filled sac that protects the lateral hip muscles become inflamed. This can occur for a variety of reasons from trauma to chronic repetitive stress injuries. Conservative management can be very effective in reducing symptoms and restoring full function.
The hip joint can become dysfunctional for a variety of reasons but when the hip capsule and its associated ligaments become very tight and restricts motion, pain will ensue. Many times the pain is either in the front or lateral portion of the upper thigh. Pain can also be referred into the groin. Improving the elasticity of the hip capsule and appropriate exercises can eliminate symptoms and restore full function.
Piriformis Syndrome is an entrapment neuropathy in which a tight and/or inflamed piriformis muscle compresses the sciatic nerve, the largest nerve in the body, producing radicular type of symptoms. There are many causes of this problem to altered foot biomechanics to poor hip joint function. Prolonged sitting and exercises that promote hip flexion and extension repetitively can create these symptoms. Although this mimics sciatica caused by a lumbar disc bulge or herniation, this syndrome is quite different in that the source of pain is the deep gluteal muscle, not the spine. There may, however be instances where a patient has both a spine issue and/or a piriformis syndrome. Once identified correctly, this can be treated conservatively with excellent outcomes.
Sacroiliac joint pain can be very severe and easily confused with lumbar disc pain based on the typical referral pattern of pain, often down the posterior thigh. It is also the most common culprit in low back pain in pregnancy. Pain is often worse with a sit to stand motion, walking or stairs and generally better with rest. The SI joint needs to be able to provide optimal stability for the pelvis while also providing an essential amount of motion. SI joint pain can be caused by a variety of muscle imbalances in the lumbopelvic region, or even in the lower extremity. For example in many patients, the larger gluteal muscles (which cross the SI joint at nearly a 90 degree angle) provide an insufficient amount of stability for the joint, while the smaller hip external rotator muscles (which cross the joint line, below the SI) are over active. This can cause compression on the lower SI preventing optimal movement. Other patients, possibly a runner, could have insufficient movement and thus force dampening occurring at the foot and ankle which causes the force to move up the leg and may cause compression at the SI joint, restricting its movement. SI joint dysfunction requires a multifaceted treatment approach that starts with an accurate diagnosis including appropriate diagnostic imaging with a goal of not just figuring out the “what” but also the "why." Treatment would typically include and functional rehabilitation program, appropriate soft tissue treatment with Graston or other forms of myofacial release, joint manipulation or mobilization and patient education.
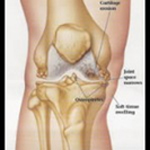
Arthritis has been used to describe chronic irritation, inflammation and degeneration of a joint. However, arthritis is broken up into two groups: inflammatory and degenerative. Inflammatory arthritis produces excessive swelling of the joint and can lead to pain and erosive changes in the joint if left unchecked.
Degenerative arthritis, as the name implies, is a wearing down of the cartilage used to protect the joint. While this does not produce any significant swelling, pain will occur through the friction that occurs when the cartilage has worn away and liberation to the joint is lost. The degenerative changes will cause stiffness in the joint, which is worsened with waking up in the morning due to lack of movement to the area overnight.
The goal of treating degenerative arthritis is therefore to increase flexibility, joint mobility, and improve surrounding musculature function to the area without further irritation. The goal of treating inflammatory arthritis is, first and foremost, to temporarily reduce inflammation to the area, followed by a plan for helping to prevent the inflammation from re-occurring. As arthritis patients will have pain in the surrounding tissue, a therapeutic plan should be addressed to lend relief and support of the affected area. Conservative treatment can have profound effects on decreasing symptoms and improving function.
The iliotibial band is a thick band of tissue that extends from the thigh down over the knee and attaches to the tibia. When the knee bends (flexion) and straightens (extension), the iliotibial band slides over the bony parts of the outer knee (lateral femoral epicondyle).
The term iliotibial band friction syndrome (ITBFS) refers specifically to a syndrome of lateral knee pain related to irritation and inflammation of the distal portion of the iliotibial band at, or just distal to, the point at which it crosses the lateral femoral epicondyle.
Iliotibial band friction syndrome is an overuse injury caused by repetitive friction of the iliotibial band across the lateral femoral epicondyle. It is a well-recognized cause of knee pain in runners, so it is commonly called “runner’s knee,” although the condition is not unique to runners, nor is lateral knee pain the only manifestation of iliotibial band injury.
It is now frequently seen in cyclists, weight lifters, skiers and soccer players. It has also been found that injury to the iliotibial band and related structures may be noted as lateral “hip” or lateral thigh pain, as well as lateral knee pain.
When evaluating for ITBFS, examining the lower back, specifically the sacroiliac joints as well as the feet is an important consideration. Conservative management will typically resolve this condition.
Your body has sacks of fluid located in strategic places to allow your tendons to effortlessly glide over your bones. If you did not have a bursa, your joints would be painful with every movement. However, sometimes this sack of fluid becomes inflamed from either an injury (such as a direct blow to the knee), overuse (such as kneeling to scrub floors) or infection.
When the bursa becomes inflamed, doctors add the ending “itis,” meaning inflammation. Thus, your bursa becomes bursitis. Usually bursitis produces a very specifically located swelling on your knee. Pes Anserine Bursitis is swelling located on the inside (medial) part of your knee along the upper part of your tibia. The pain of bursitis is usually sharp and worse with either touching the area or even when you sleep and the two knees touch each other. This typically happens in older patients.
Patellar bursitis (or “pre-patellar bursitis”) is located over the front of the patellar ligament and kneecap (patella) – see the picture to the right. The pain is located right in the front of your knee, and it can even be painful to have the bed sheets touch your skin in this area. This is the most common type of bursitis. An infection to the bursa usually has redness associated with this swelling, and the pain is constant. Conservative management is very effective in helping these conditions.
A knee sprain means that you have injured one of the ligaments in and/or around the knee joint. A sprain is caused by a ligament being stretched too far. The symptoms of a sprain are typically pain, swelling, and bruising of the affected joint. The collateral ligament sprains will affect lateral stability and the cruciate sprains will affect stability in the frontal plane. Many knee sprains can be treated conservatively however if there is significant instability, there may need to be surgical intervention.
Injury to one of the two crescent-shaped cartilage pads between the two joints formed by the femur (the thigh bone) and the tibia (the shin bone) is Meniscal injury. A partial or total tear of a meniscus may occur when a person quickly twists or rotates the upper leg while the foot stays still (for example, when dribbling a basketball around an opponent or turning to hit a tennis ball). After any injury the knee may click, lock, or feel weak. Symptoms of meniscal injury may disappear on their own but frequently, symptoms persist or return and require treatment.
Your joints move by the power of your muscles. The muscles attach to your joints through tissues called tendons. The tendons transfer the force from your muscle across the joint and cause it to move. Sometimes this tendon becomes inflamed because it was injured (such as a direct blow to the thigh) or overused (such as biking up hills).
When the tendon is inflamed, doctors add the ending “itis,” and thus, we call this Tendonitis/Tendonosis.
Chronic cases are called tendonosis, indicating chronic inflammation. In some cases, the tendon actually tears in half, and this is called a tendon rupture. If you can’t straighten your knee because of pain over your tendons, seek immediate medical treatment.
Tendonitis/Tendonosis pain is usually described as an ache that can be sharp with exiting from a chair or with squatting. The pain is usually improved with rest. Usually the patellar tendon in the front of your knee is most involved. This is called “patellar Tendonitis/Tendonosis” or “jumper’s knee.” This syndrome is frequently caused by imbalances of the knee muscles and hip muscles causing the knee cap to “track” incorrectly. Further, biomechanical issues in the foot can be a contributing factor. This pain is usually located over the front of your knee and is described as a deep aching pain. It is sometimes associated with swelling and is usually worse when your knee is bent for long periods of time such sitting in a car or bus.
The pain is also worse with such activities as running, biking, squatting, kneeling or stair climbing (either up or down stairs).
It is sometimes associated with mild or moderate swelling of the knee and some people report a grinding feeling in their kneecap. It is more common in younger females especially after a growth spurt where the knee must carry more weight.
This causes irritation and inflammation on the undersurface of the knee cap and ultimately cartilage degeneration.
Identifying the causes of the pain and inflammation and directing functional treatment have very good outcomes for these conditions.
This is a very common condition for people of all activity levels, but especially those who are active through running, walking, or sports. The Achille’s Tendon is the largest tendon in the lower leg and is the end of the gastrocnemius and soleus muscles in the calf as they insert onto the heel bone. The calf muscles, when they contract, cause the toes to point (like a ballerina). Their most important job is to propel the body forward when walking or running or propel it upward for jumping. Unfortunately, if the tendon is weakened, then repeated contraction of the calf muscles through these activities will cause pain. The pain can be anywhere in the calf, but is most commonly in the calf musculature itself or in the tendon down toward the heel. The pain can be a burning-type or a soreness or even feel like a cramp is going to happen (or has happened) in the calf.
This condition is best treated using Graston® Technique to restore the strength of the tendon and with Funhab® to improve the strength of the calf musculature. In addition, Kinesio® Taping Method commonly helps to assist the tendon in performing its job with less pain.
Ankle sprains are very common. They occur when the forces imparted onto the patient are too great for the ligaments to hold their tensile strength. There are three grades to lateral ankle sprains, whereby either one, two or three of the ligaments of the ankle are torn. The most common ligament in the ankle to tear is the anterior talofibular ligament. This is where we “roll” our ankle. Conservative management is very important not just to decrease pain and inflammation but to restore function. An ankle brace alone with no other therapy may have an increased likelihood of repeatedly spraining the ankle.
A condition that occurs when there is chronic inflammation to a large band of tissue on the bottom of your foot called the plantar fascia.
Because this fascia is on the bottom of your foot, doctors call this area the plantar surface, meaning sole of the foot in Latin. The purpose of this ligament is to help support the arch of your foot. When this fascia becomes inflamed, doctors add the ending “itis” thus, the term plantar fasciitis. Sometimes, on X-rays, a heel spur is seen; however, it is not the cause of your pain. Numerous scientific studies have shown that the plantar fascia is the primary source of pain (i.e. don’t let anyone talk you into surgery to remove the heel spur).
The cause of this condition is not fully understood, but it is more commonly found in females and overweight people. When both feet are involved, this is sometimes associated with a certain type of arthritis, which can be evaluated with a simple exam and tests by your doctor. This problem can often be caused by a heel cord (achilles tendon) that is too tight.
The pain occurs on the bottom of your heel, usually more toward the inside (“medial”). It hurts to take a step or walk. Most patients report that the pain is worst when getting out of bed in the morning. The pain usually gets better after walking around for a while. The reason the pain is worst in the morning is because the plantar fascia has had the chance to contract (shorten, tense up) all night long while you are sleeping.
The pain can be described as a sharp pain (like stepping on a pebble) or a dull aching/throbbing pain. Plantar fasciitis is very common, but is easy to treat WITHOUT SURGERY.
Shin splints, the common term for anterior or posterior tibialis syndrome, presents as pain along the tibia (front of shin) in the muscles or bone itself. The pain is caused by small tears in the muscles that attach to the tibia and usually results from vigorous physical activity. It is most commonly seen in runners. Appropriate conservative treatment typically can resolve the problem. If not managed appropriately, this condition can progress to a tibial stress fracture.